The Gut-Brain Connection and Your Depression
Is This The Missing Link?
When my son had depression and I look back now, it all makes sense. But it didn’t make sense to me back then. I did not know anything about the gut-brain connection.
He had GI issues from the time he was born but then while he was still a toddler it seemed to subside. Around 5th grade he started to get sick again, lose weight, had mono, was tested for celiac, had GERD and on and on it went for a while with many specialists and no answers.
I wish I had known what I know now because I think if we addressed all his gut issues early on, he never would have had to suffer with debilitating depression.
But I didn’t know about the gut-brain connection. You see his gut was in very bad shape and that eventually affected his brain health.
But don’t think, “I don’t have gut or digestive issues so my gut must be fine. My gut-brain connection is not a concern for me”.
Please don’t think this way and read on.
Did you know that what affects your gut can affect your brain? I know it sounds crazy, but if you have GERD, low HCL, IBS, IBD, intestinal permeability, food sensitivities, poor diet, medication use, birth control use and much more, all of this can all impact your gut.
Maybe you take ibuprofen, or were on birth control pills, or drink diet soda every day or are eating foods that cause inflammation (only you don’t know it), or you have been under a great deal of stress from school, work, family or friends.
Your gut may feel fine. But did you know that what I just mentioned (and much more) can impact your gut health without you even knowing it. And when gut health is disrupted, so too can your brain be disrupted.
That’s right. When your gut is impacted so is your brain.
This does not mean that everyone with poor gut health has depression. Some may have brain fog, forgetfulness, ADD/ADHD, anxiety, irritability, anger, moodiness, dementia and so forth. The odds are if you have gut issues your brain is not at its optimal health whether you realize it or not.
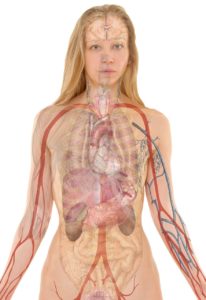
The Gut-Brain Connection
You may have heard in your research on depression that the gut is called the second brain. Some in the health field now even call the gut the “first brain”.
The vagus nerve connects the gut to the brain. Scientists have known about the gut-brain connection for over a hundred years. They first studied the effect that stress and mood can have on gastric physiology. Thus, they were aware of the brains ability to control gut function, but it took longer to learn that this was not a one way street but a two was highway. Research has now shown that the gut microbiota health can be linked to behavior, and mood disorders.
For instance, when you are nervous and must give a public presentation, you may feel “butterflies” in your stomach. This is the signaling going from the brain to the gut. But if you eat a poor diet, and have very little good bacteria in the gut and very few strains, this can cause inflammation. But this inflammation may not be isolated to the gut and can cause brain inflammation as well.
Even some of your neurotransmitters, such as your serotonin, which is known as the “feel good” neurotransmitter, is made up mostly in the gut and travels via this vagus nerve. Serotonin synthesis occurs in the gut neurons and within the neurons of your brain stem. For your serotonin production to occur, it needs tryptophan (a precursor to serotonin) to gain access to the central nervous system via the blood brain barrier. Tryptophan competes with other amino acids for transport to the brain. Other factors also influence how much tryptophan gets eventually converted into serotonin. Without going into serotonin and your gut-brain connection, just know for now that having good gut health is important for neurotransmitter production and function.
This may be overwhelming to you like it was for a client of mine. When I first told her that her depression was related to her gut, she broke down and cried and said “I don’t know what to believe. You are telling me I need to look to my gut and my doctor tells me it is all in my head”.
If you have doubts, like she did, I encourage you to look at the sources I have listed and look at more research done in this area. Also, ask yourself, if you doctor said it is all in your brain, is what the doctor is doing for treatment helping? Maybe it is, but it only slightly and not at all or with many side effects, you may want to look deeper.
Your Gut Bacteria and Its Impact On Your Brain
Bacteria, the good and the bad make up your gut microbiome. Not only can certain health issues, and diet and lifestyle factors affect your gut health, but it can impact the type of bacteria that you have. This is very important because research has found that they type of bacteria you have can impact your mood, behavior and emotions.
While you may not think bacteria in your gut is such a big deal, it really is. In fact we have more bacteria than we do our own cells. Your bacteria can weigh in total up to five pounds and is a ecosystem in you that impacts your physical and mental well-being.
Our gut microbiome starts at birth and it has its biggest impact on the brain early in life. While your gut microbiome is unique to you, you get your bacteria from your mother and as you pass through the birth canal (for a vaginal birth). Unfortunately your birth microbiome was out of your control. And don’t blame your mother as she didn’t know how important gut health is to her baby. I know I didn’t know anything about this, and certainly my mother who was stressed in my pregnancy did not have any clue about how her health impacts her baby.
I call this your “constitution”. Some people are born with stronger constitutions than others. What I mean by this, is that some babies are healthier right from the “get go” because their birth microbiome is healthier. But even so, those with strong birth constitutions can have a disrupted gut microbiome later in life. And vice versa, those with poor birth constitutions can take measures to improve their microbiome over their life time.
Research has found that tweaking the balance of good and bad gut bacteria can alter your brain chemistry. Which way your brain chemistry goes would depend on if you are tweaking the good bacteria or the bad.
If you are under a great deal of stress, this can cause a shift in the bacteria balance.
Therefore, by altering the gut microbiome and improving the types of gut bacteria you have, can alter and benefit your mood.
Remember the vagus nerve and the highway I mentioned above? You want all the cars on that highway flowing with no accidents, no traffic. You want the communication to flow through the vagus nerve easily back and forth.
Restoring Gut Health
It is one thing to start eating probiotic and prebiotic rich foods or taking a probiotic supplement but the question is “what caused the shift in the microbiome in the first place?”. Did it happen at birth, or from stress, from antibiotics, NSAIDS, head injury or diet or an autoimmune condition?
The point I am making is that, probiotics are great, I take them myself, but if you don’t address what caused the shift then what’s the point in taking another supplement? On top of this, a probiotic may not be what you need right now or you may need additional support for gut health. This is where an individualized approach comes into play to address you and your health and your depression instead of a pill for every ill.
Bottom Line: Find out if you have a gut issue (we can test) and then determine what is causing your gut issue and address it in order to support optimal brain health.
What do you think? Do you think depression is all in your head or does the gut-brain research sound plausible to you? I would love to hear your thoughts! Please comment on what you think.
Sources
http://www.apa.org/monitor/2012/09/gut-feeling.aspx
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3788166/
https://www.nature.com/news/gut-brain-link-grabs-neuroscientists-1.16316
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4662178
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4748667/

Leave A Comment
You must be logged in to post a comment.